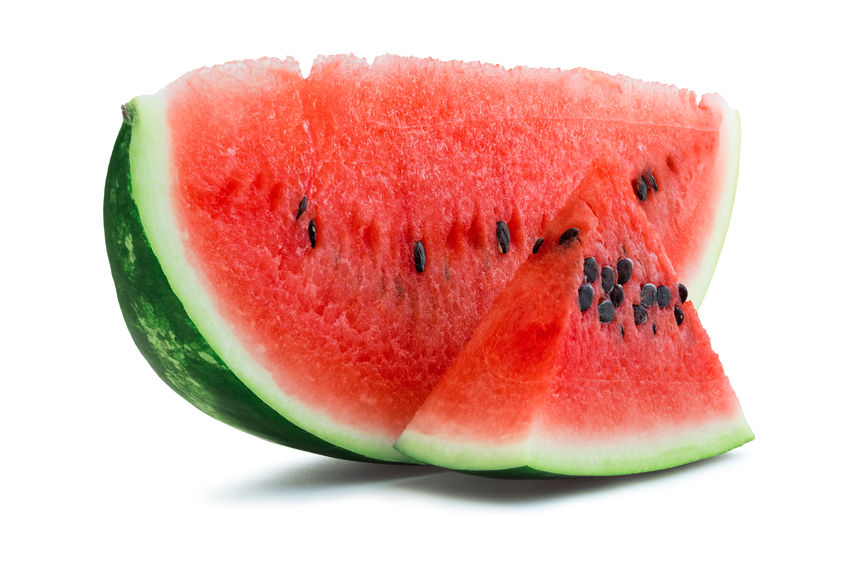
COVID-19 health risk estimate*
Politicians are urging us to return to normal. This is designed to save the economy but may harm public health or public death. So, as things open up, can you use your personal health history to decide when or if to return to stores, malls, restaurants etc.? Check chart at right total your score, see recommendations below*. Always check with your healthcare professional before changing any treatment plan.
*Please note that my assessment is not approved or even reviewed by the CDC or any official organization. It is simply a suggestion that can be used to determine how much to move back into economic activity based on an estimate of your own risk. Nothing on this web site is to be used to cure or treat any disease or illness.
- If your score is 0, the risk of serious COVID 19 illness is that of the general population.
- If your total score is 1–4 your risk of serious COVID 19 illness is higher than the general population. Caution is recommended e.g. wear a mask, avoid large groups, social distance at open restaurants, wash hands frequently.
- If your risk is 5 or greater you are at very high risk of serious disease and death. Even more extreme caution is recommended e.g. wearing a mask, avoid as much public contact as possible, wash hands, stay at home, avoid open restaurants, use telemedicine doctor’s appointments.
Cheaper Insulin??
Insulin cost has increased more than 500% over the past several years. This ridiculous cost surge is being addressed, at least  partially, by the major insulin manufacturers in view of current economic circumstances.
partially, by the major insulin manufacturers in view of current economic circumstances.
Eli Lilly. People who have commercial insurance or if no insurance, a monthly prescription can be had with a $35 co-pay for many of insulins, e.g. Humalog, Humalog 75/25. See LillyCares Here
Novo Nordisk. For $99, people with diabetes can get up to three vials or two packs of FlexPen®/FlexTouch®/PenFill® pens, or any combination of Novo Nordisk Inc. insulins with a prescription. “Medicare Part D beneficiaries must agree to obtain their Covered Insulins subject to this offer throughout the entire applicable Part D coverage year, if Part D coverage would otherwise be available.” NovoLog; NovoLog Mix 70/30; Levemir; Tresiba; Fiasp; Novolin in; Novolin R; Novolin 70/30. See requirements here. Apply here
Sanofi. Possible eligibility if medication not covered by insurance. One may be eligible with Medicare part D if the plan does not cover your medication.
Toujeo: pay as low as $0 up to $99 for a 30-day supply, depending on insurance coverage. Maximum savings apply. Valid up to 10 packs per fill; Offer valid for one fill per 30-day supply
Lantus: pay as low as $0 up to $99 for a 30-day supply, depending on insurance coverage. Maximum savings apply. Valid up to 10 packs per fill; Offer valid for one fill per month per 30-day supply
Apidra: pay as low as $0 copay with maximum savings up to $100 per pack, up to 1 pack per fill;
Soliqua 100/33: pay as low as $0 copay with maximum savings up to $800 per pack, up to 1 pack per fill. See requirements here.
Details on insulin help programs from the American Diabetes Association. Here.
 Depression in diabetes and thyroid disease.
Depression in diabetes and thyroid disease.
Several studies indicate a person with diabetes is more likely to be depressed, as much as 2 -3 times more likely. There is also an increase in risk of diabetes in people who are depressed.
Nearly 70% of people with an overactive thyroid have depression. An underactive thyroid produces symptoms that mimic depression but may simply be a symptom of the disease.
Definitions of depression are controversial. The American Psychiatric Association defines it like this: “Depression (major depressive disorder) is a common and serious medical illness that negatively affects how you feel, the way you think and how you act.”
What is it like?
It’s like drowning, except everyone around you is breathing (psycom.net).
It’s like running in a deep ditch in front of a flash flood. You can’t stop, you think you know how to get out but can’t seem to do it.
There is no way out, no light at the end of the tunnel.
You are on a train headed for disaster and have no way to stop it.
I spite of your best efforts sh*t happens.
Signs and Symptoms
If you are experiencing some of the following signs and symptoms most of the day, nearly every day, for at least two weeks, you may be suffering from depression (according to the National Institute of Mental Health):
Persistent sad, anxious, or “empty” mood.
Feelings of hopelessness, or pessimism.
Irritability.
Feelings of guilt, worthlessness, or helplessness.
Loss of interest or pleasure in hobbies and activities.
Decreased energy or fatigue.
Moving or talking more slowly.
Feeling restless or having trouble sitting still.
Difficulty concentrating, remembering, or making decisions.
Difficulty sleeping, early-morning awakening, or oversleeping.
Appetite and/or weight changes.
Thoughts of death or suicide, or suicide attempts.
Aches or pains, headaches, cramps, or digestive problems without a clear physical cause and/or that do not ease even with treatment.
Not everyone who is depressed experiences every symptom. Some people experience only a few while others may experience many.
Diabetes and depression work hand in hand. It is difficult to do the things to take care of diabetes while depressed. Depression takes away the urge to test blood sugar, take medications and insulin, the diabetes is therefore likely to be worse. Elevated blood sugar worsens the mood, reduces energy, induces difficult sleeping and sleep apnea. Comfort food is often high in carbohydrates and fat making diabetes worse. A failure to take thyroid medication causes anxiety and /or depression
What to do?
- Move toward things that increase self-esteem. Migrate to those things that you do well e.g., if you are good and arts and crafts do more of that.
- Take your medication event if it costs too much and you just don’t feel like it.
- Good examples are Zumba, group sports. Try to find an exercise partner. Studies show that the exercise is likely to be continued if there is another person helping with the motivation.
- Eat healthy 1.
- Get enough sleep.
- Get tested for diabetes and thyroid disease.
Not sure if you are just blue or really depressed? Take a test here. I took this test and it indicated I have moderate depression and “If you notice that your symptoms aren’t improving, you may want to bring them up with someone you trust.”
When to seek help
If symptoms of depression are causing problems with relationships, work, or
family — and there isn’t a clear solution — you should see a professional.
Seek emergency services (911) if there are warning signs of suicide, e.g.:
Talking about wanting to die or to kill oneself;
Looking for a way to kill oneself;
Talking about feeling hopeless or having no purpose;
Talking about feeling trapped or being in unbearable pain;
Talking about being a burden to others;
THC and CBD oil in diabetes
There are many points of view on the use of marijuana and or cannabidiol. The view is often dictated by whether the person starts out “fur it or agin it”.
THC
Clinical studies from major universities are generally trustworthy. One can’t have a point without a point of view. It is estimated that 10 to 15% of University professors smoke pot. Nevertheless, there are  several large studies including one from the University of Minnesota with evidence that marijuana smoking decreased the risk of diabetes and the metabolic syndrome but increased the risk of pre diabetes. How does one figure that?
several large studies including one from the University of Minnesota with evidence that marijuana smoking decreased the risk of diabetes and the metabolic syndrome but increased the risk of pre diabetes. How does one figure that?
Smoking anything is likely to increase the risk of lung disease. There are studies that smoking THC increases the risk of heart attack but that’s probably less related to the THC than the smoke.
CBD
THCV and CBD cannabinoids may increase sensitivity to insulin according to Adrian Devitt-Lee, a chemist involved in cannabinoid research who is employed by a medical cannabis producer. Others indicate such evidence. The concern with CBD in diabetics taking insulin is increased risk of low blood sugar. There are studies showing a decrease in pain of peripheral neuropathy with CBD oil. An increase in the effectiveness of nonsteroidal products such as ibuprofen has been shown.
Below is a direct quote on the current state of evidence and recommendations for research by a committee of the National academies of Sciences, Engineering and Medicine from January 2017.
“There is conclusive or substantial evidence that cannabis or cannabinoids are effective:
- For the treatment for chronic pain in adults (cannabis)
- Antiemetics (anti-nausea) in the treatment of chemotherapy-induced nausea and vomiting (oral cannabinoids)
- For improving patient-reported multiple sclerosis spasticity symptoms (oral cannabinoids).
There is moderate evidence that cannabis or cannabinoids are effective for:
- Improving short-term sleep outcomes in individuals with sleep disturbance associated with obstructive sleep apnea
syndrome, fibromyalgia, chronic pain, and multiple sclerosis (cannabinoids, primarily nabiximols).
There is limited evidence that cannabis or cannabinoids are effective for:
- Increasing appetite and decreasing weight loss associated with HIV/AIDS (cannabis and oral cannabinoids).
- Improving clinician-measured multiple sclerosis spasticity symptoms (oral cannabinoids).
- Improving symptoms of Tourette syndrome (THC capsules).
- Improving anxiety symptoms, as assessed by a public speaking test, in individuals with social anxiety disorders (cannabidiol).
- Improving symptoms of posttraumatic stress disorder (nabilone; one single, small fair-quality trial).
There is limited evidence of a statistical association between cannabinoids and:
- Better outcomes (i.e., mortality, disability) after a traumatic brain injury or intracranial hemorrhage.
There is limited evidence that cannabis or cannabinoids are ineffective for:
- Improving symptoms associated with dementia (cannabinoids)
- Improving intraocular pressure associated with glaucoma (cannabinoids).
- Reducing depressive symptoms in individuals with chronic pain or multiple sclerosis (nabiximols, dronabinol, and nabilone).
MY CONCLUSION: there is simply not enough good hard clinical evidence one way or the other on CBD oil and THC. More studies are needed. Considering that 19 million Americans currently use marijuana and the increasing popularity of CBD oil, more information should be forthcoming.
Are you taking fewer insulin doses than prescribed?
One study showed only 63% of prescribed doses were being taken by patients with type 2 diabetes. Other studies show a higher A1C based on missed doses.
Reasons we frequently hear are: eating out, can’t comfortably inject at work or just plain forgot.
So, what are options?
Type 1 diabetes 
Insulin pump
Inhaled insulin plus 1 basal insulin injection
Type 2 diabetes
V-Go
Insulin pump.
Inhaled insulin plus pills or 1 basal insulin injection
The V-Go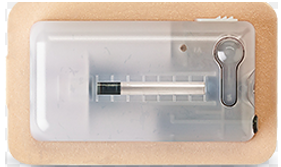

Pros
Small (about 1¼ x 2 ¼ x ¼ in deep).
Can be worn any place insulin can be Injected.
Lasts 24 hours
One insulin covers all insulin needs (1 co-pay 😊)
Cons
Must be changed daily
Dose is limited by the model V-Go used.
Device must be filled with insulin
Got Gout? Got Diabetes AND Gout?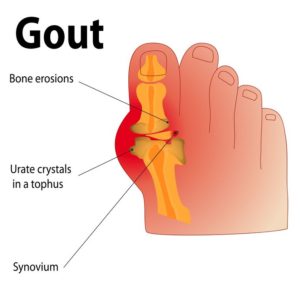
Did your gout get better after having diabetes?
Gout occurs in about 4% of the US population. It is a form of arthritis resulting from crystal deposits in joints and surrounding tissues. The result is pain, swelling, tenderness and warmth.
A person with gout is more likely to develop type 2 diabetes but a patient with diabetes is less likely to have gouty attacks. This may be because increased urine flow to get rid of sugar in diabetes may also get rid of uric acid. Also, metformin may have an anti-inflammatory effect.
Elevated blood uric acid must be present for gout to develop but most people with elevated uric acid never develop gout. The risk of developing gout is increased by being an older male, African-American or Pacific Islander. Gout occurs in all groups, however.
Once a person has had a gouty attack, some things make it more likely to happen again.
Traditionally gout was considered a rich man’s disease because of the wealthy could afford “rich” foods likely to increase uric acid.
Alcohol–decreases urine excretion of uric acid.
Food–any that are high in purines. These include organ meats like liver, seafood like sardines, salmon and some vegetables including spinach (see list).
Medicines–these include diuretics, beta-blockers even low-dose aspirin.
Chronic kidney disease reduces excretion of uric acid.
NON-MEDICAL TREATMENT
Some foods have been shown to reduce uric acid levels and lessen gout attacks.
Coffee–regular and decaffeinated.
Vitamin C.
Cherries.
Medications for gout
Colcrys TM(colchicine) – Anti-inflammatory ,decreases swelling and the buildup of uric acid crystals.
NSAIDs (Nonsteroidal Anti-Inflammatory Agents) e.g. ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Continuous use is not recommended in diabetes because of possible kidney damage.
Corticosteroids. These are the best anti-inflammatory agents but may markedly increase blood sugar in folks with diabetes, increase blood pressure and others. Steroids are generally reserved for those and cannot take colchicine (Colcrys TM) or NSAIDs
Avoid these foods if possible for gout
Foods with very high purine levels: | Anchovies, Brains, Gravies, Kidneys, |
Foods with high purine levels: | Bacon, Beef, Calf tongue, Carp, Chicken soup, |
Foods with moderately high purine levels: | Asparagus, Bluefish, Bouillon, Cauliflower, |
Is my medicine making me fat? The short answer is YES, but the biggest issue is hands to mouth syndrome.
Gasoline is fuel for your vehicle, FOOD is fuel 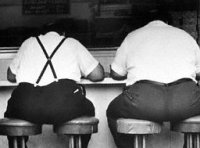 for your body. If you put in more than you use, the overflow must go somewhere. If you eat more than you burn, the body has nothing to do with it but store some away for a rainy day. Most of us never see that food-free rainy day. We hear “I just can’t lose weight”, well, did you ever see an image of a fat starving person?
for your body. If you put in more than you use, the overflow must go somewhere. If you eat more than you burn, the body has nothing to do with it but store some away for a rainy day. Most of us never see that food-free rainy day. We hear “I just can’t lose weight”, well, did you ever see an image of a fat starving person?
Once there is too much of you, everything and everybody seem to work against shedding some pounds. Food ads, stress, sin, medicines, arthritis to name a few. The body likes to maintain the fat it’s been living with all these years. If you reduce fuel intake, it will shift metabolism and get more miles to the gallon. Despite all of this, you can’t fail to lose weight if you take in less than you burn.
Insulin and drugs that stimulate the pancreas to secrete insulin enable use of carbs that might otherwise be eliminated in urine. Mild drops in blood sugar makes you feel hungry. Anti-psychotic and antidepressant drugs increase appetite and makes one feel more like eating.
Diabetes medicines linked to Weight loss
exenatide (Byetta/Bydureon)
liraglutide (Victoza, Saxenda)
lixisenatide (Lyxumia)
albiglutide (Tanzeum)*
dulaglutide (Trulicity)
semaglutide (Ozempic)
* not available in US and UK but is available in India.
Diabetes medicines linked to Weight gain
Insulin
Very rapid-acting (Afrezza)
Rapid-acting (Apidra, Humalog, Admelog, Novolog)
Short-acting (Regular, Humulin-R, Novolin-R, Reilon-N)
Intermediate-acting (NPH, Humulin-N, Novolin-N, Relion-N, Humulin R u500)
Long-acting (Lantus, Basaglar, Toujeo, Levemir, Tresiba)
Pre-mixed (Humulin 70/30, Novolin 70/30, Novolog 70/30, Humulin 50/50, Humalog mix 75/25)
Sulfonylureas
DiaBeta, Glynase, or Micronase (glyburide or glibenclamide)
Amaryl (glimepiride)
Diabinese (chlorpropamide)
Glucotrol (glipizide)
Tolinase (tolazamide)
Tolbutamide.
Meglitinides
Repaglinide (Prandin)
Nateglinide (Starlix)
INSULIN. Everything going on inside the body and its surroundings make for changes in blood sugar.
While multiple organs are responsible for increased sugar, the liver and the mouth are big players. Liver and other organs produce sugar at steady rate, we call that background or “BASAL” sugar. Therefore, one needs BASAL insulin for this constant production of sugar. Food comes intermittently or in in a BOLUS, so one needs BOLUS insulin for that. The multiple doses of insulin and then called BASAL/BOLUS. Basal insulin is long acting, and bolus insulin is short or rapid acting.
Examples of basal insulin are: Lantus®, Levemir®, Toujeo®, Tresiba® and Basaglar®.
Examples of short acting (rapid) insulins are Afrezza®, Humalog®, Novolog®, Apidra®, Fiasp®.

Afrezza®, the only currently available inhaled insulin is rapidly absorbed, more so than injected insulin. It has several advantages over injected insulin.
It decreases the risk of low blood sugar because it is effective in 12 to 15 minutes and is gone in 180 minutes.
It is painless, convenient and effective. It is released into the bloodstream through the lungs .
Blisters of insulin are color-coded making it easy to identify the number of units to use. Blue is for 4 units, green is for 8 units and yellow is for 12 units of insulin. The color coding reduces the possibility of mistakes.
The inhaler is small, not necessarily noticeable in a crowd and can be easily carried in a pocket or purse.
The inhaler is included in the monthly prescription.
It is easy to use.
I personally use this product at meal time or if blood sugar is elevated. Recently I was prescribed a steroid which of course INCREASES blood sugar. I was able to inhale 4, 8 or 12 units every 2 hours because two thirds of the is out of the system within 120 minutes. I therefore did not have to worry about insulin stacking and going low. It is a short acting insulin and must be used with a basal insulin such as Lantus®, Levemir©, Toujeo®(glargene U300), Tresiba ®(degludec).
The major downside is a mild cough caused by the powder striking the back of the throat. Cough can be minimized by taking a sip of water before and after the inhalations. Otherwise the downsides are like any other insulin.
There is common agreement that good “control” of diabetes reduces risk of complications. Type 2 diabetes gets worse with time. There may be no symptoms in early stages of worsening. How does one know if complications are silently developing? The only way to know is some sort of testing. Common tests include:
Hemoglobin A1c
Pros:
- A1c is an indicator of average blood sugar over the preceding 6-12 months. Important diabetes studies use A1c to predict complications and medication effectiveness.
Cons:
- It only gives an average. If sugar is up and down severely, the average may be at target, but patient may be exposed to dangerous lows or highs.
- There are generally no symptoms as T2 diabetes gets worse. If A1c is the only thing tested, one might delay discovery of poor control.
- Anything changing red blood cell life can make A1c false. Recent blood loss, sickle cell disease, other inherited hemoglobin variants, hemodialysis, transfusion, vitamin B-12/folate deficiency anemias, and spleen removal.
- Different methods of A1C testing vary in accuracy and susceptibility to interference.
Finger stick testing:
PROs
- Immediate feedback of current blood sugar.
- Used appropriately it is a great educational tool to measure the effects of food, exercise, stress, etc. on blood sugar.
CONs
- Painful
- Expensive
- Possible excessive bleeding
- Slight risk of infection
- Scarring
- Many cheaper meters/strips are inaccurate
- Inaccuracy caused by improper cleansing of the area to obtain blood, e.g. small amounts of a sugary substance or liquid left on the finger.
How often should one test?
Fingerstick testing should be done as often as needed to determine current blood sugar and to reach target diabetes control. No one rule fits everyone. One is best suited to follow the directions of your diabetes treatment team.
Below are guidelines used by the Diabetes Control Center. Our guidelines are NOT to be used in place of directions of your personal medical professional.
Applies only to controlled diabetes
Diabetes state | Testing frequency |
Pre-diabetes | 1 x / mo.1 |
T2 DM controlled by diet | 1 – 3 x /mo.1 |
T2 DM pill(s) (not SU)2 | 1 – 3 x /wk1 |
T2 DM pill(s) (SU)2 | 1 – 2 x/day |
T2 DM pill(s) + basal insulin3 | 2 – 3 x/day |
T2 DM basal + mealtime insulin | 3 – 4 x/day |
T1 DM | 4 – 8 x/day |
1Infrequent testing is best done 2 hrs. after the largest meal – target 140mg or less.
2SU (sulfonylurea drugs like glipizide, glimepiride or repaglinide, nateglinide).
3Basal, long acting insulin like Lantus, Toujeo, Tresiba, Basaglar Levemir
 Go to a clinic for your neuropathy pain? Not recommended. The treatment for diabetic polyneuropathy is control of diabetes. Our patients with severe diabetic polyneuropathy have had good relief after reaching target A1C levels. Improvement in diabetic polyneuropathy can take up to 90 days after good control is reached. In the meantime, the patient has severe, sometimes debilitating pain. We use temporary treatment with drugs like Gabapentin or Lyrica until control of diabetes is reached. These drugs were developed for epilepsy, the exact way in which they work is not known. Their action seems to involve the transmission of impulses in the nerves. The problem is they don’t know the difference between the nerves in your feet and the nerves in your head. Dizziness, drowsiness and low energy therefore are common side effects.
Go to a clinic for your neuropathy pain? Not recommended. The treatment for diabetic polyneuropathy is control of diabetes. Our patients with severe diabetic polyneuropathy have had good relief after reaching target A1C levels. Improvement in diabetic polyneuropathy can take up to 90 days after good control is reached. In the meantime, the patient has severe, sometimes debilitating pain. We use temporary treatment with drugs like Gabapentin or Lyrica until control of diabetes is reached. These drugs were developed for epilepsy, the exact way in which they work is not known. Their action seems to involve the transmission of impulses in the nerves. The problem is they don’t know the difference between the nerves in your feet and the nerves in your head. Dizziness, drowsiness and low energy therefore are common side effects.
Diabetes is a common cause of polyneuropathy, but it is not the only cause. Polyneuropathy has several causes ranging from diabetes, alcohol abuse, HIV and other infections, medications, untreated hypothyroidism, vitamin deficiency, toxins, infections and hereditary factors. My problem with some of my colleges is the attitude, “you’ve got foot pain and you’ve got diabetes, that’s that, nothing can be done.” If diabetes is in control but neuropathy symptoms continue, it’s important to look for other causes.
Quotes from the Foundation for Peripheral Neuropathy
“Patients seeking treatment of peripheral neuropathy need to be aware of a recent controversial method that involves collaboration between chiropractors, medical doctors and/or podiatrists…. In most of the schemes identified, the patient will briefly see a medical doctor on the first visit. The medical doctor will order all the tests, braces and injections. He may recommend the patient undergo physical therapy and/or chiropractic care in the clinic as well. Typically, all of the localized anesthetic injections are given by a nurse. A chiropractor and/or physical therapist may render various treatments over the course of care, further increasing the cost. The patient rarely sees the medical doctor again….A typical PN scheme protocol includes expensive and sometimes painful, nerve conduction testing. These tests may be done at the onset of treatment and intermittently throughout the care program. These tests may have no basis other than to generate income for the clinic. The clinician may X-Ray the patient’s neck, back, arms, legs and feet. These x-rays have often been found to have no value in helping the doctor reach a diagnosis. The clinic also orders a variety of elastic and hard, plastic braces for the patient’s neck, back, wrists and/or ankles. In the majority of instances, these braces were found to offer little assistance to the patient’s painful condition. These supports are expensive with bills totaling over thousands of dollars. The actual treatment that the clinic renders for the peripheral neuropathy pain includes frequent (2-3 x per week) injections of an anesthetic agent, often Marcaine, into the peripheral nerves of the arms/wrists/legs/calves and/or feet. There have been instances in which patients have received over 100 treatments involving up to 5 injections per day.” To Read more from the Foundation for Peripheral Neuropathy go to (https://www.foundationforpn.org/2016/04/11/5179/).
 Are blood sugar meters accurate? Some more than others. A few years ago, I attended a conference on glucose monitoring sponsored by the American Association of Clinical Endocrinologists. Several startling points were brought out :
Are blood sugar meters accurate? Some more than others. A few years ago, I attended a conference on glucose monitoring sponsored by the American Association of Clinical Endocrinologists. Several startling points were brought out :
- The FDA does not have authority (from congress) to remove blood glucose meters from the market that don’t meet standards.
- The FDA has not updated standards for accuracy in glucose meters for more than 10 years.
- The FDA does not have permission to perform surprise manufacturing standard visits at offshore facilities providing glucose meters and strips to the United States market.
Dr. David Klonoff presented a proposal to provide a service testing and certifying the accuracy of glucose measuring devices. Fortunately to his credit, a publication recently described accuracy levels of several glucose meters on the US market.
FDA recommended standards.:
99% of meter blood sugar measurements are within 20% of lab results, or
95% of meter blood sugar measurements are within 15% of lab results
ISO (International Organization for Standardization) requirements for glucose meters:
Within ± 15 mg/dl of laboratory results at concentrations of under 100 mg/dL
Within ± 20% of laboratory results at concentrations of 100 mg/dL or more
Allowing 15% variation from lab values, this is possible:
In the study, each meter brand was tested over 300 times at 3 different sites*
Meters with 100% accuracy compliance in all 3 studies and receiving stamp of approval were:
Contour Next; ACCU-CHEK AVIVA Plus; ReliOn Confirm/micro; CVS Advanced; FreeStyle Lite; ACCU-CHEK SmartView.
Meters failing 1 of 3 tests were
ReliOn Prime; OneTouch Verio; Prodigy No Coding; OneTouch Ultra; ReliOn Ultima.
Meters failing all 3 tests were:
Contour; Embrace No Code; TrueResult: TrueTrack; SOLUS; Advocate; Gmate.
* several meters e.g. Dario (use ISO standards) were not tested.
Examples of 20% variation
| Lab | Meter High | Meter Low |
| 100 | 120 | 80 |
| 120 | 144 | 96 |
| 150 | 180 | 120 |
| 170 | 204 | 136 |
| 200 | 240 | 160 |
| 225 | 270 | 180 |
| 250 | 300 | 200 |
| 275 | 330 | 220 |
Carpal Tunnel Syndrome (CTS)
If you have diabetes and or thyroid issues plus pain or numbness in the fingers, wrist or arm, there is a good chance you have Carpal Tunnel Syndrome (CTS).
Symptoms of Carpal Tunnel Syndrome (CTS) include:
Dull aching and or numbness in the hand, forearm or upper arm
weakness in more severe situations
CTS is frequently brought on by repetitive hand/wrist motion. Some diseases are associated with it. CTS occurs in both arms about 65% of the time.
Diseases linked to CTS
- Diabetes
- Thyroid dysfunction
- High blood pressure
- Pituitary gland dysfunction
- Fluid retention or swelling from any cause
- Rheumatoid arthritis
Diagnosis
- Tinel sign
- Phalen maneuver
- The hand elevation test
- Nerve conduction tests
Treatment
- Splinting: initial treatment is usually wrist Brace worn at night.
- Avoid activities that bring on symptoms.
- Medications – Over the counter nonsteroidal anti-inflammatory (NSAIDs) medications. or prescription ones such as Meloxicam or corticosteroids.
- Surgery
Why an eye exam?
Diabetic eye disease has no symptoms at first. Nearly 30% of people with diabetes have some form of eye problems from it. The good news: early detection by a dilated eye exam with timely treatment and follow-up can prevent vision loss and blindness. A mere vision test will not cut the mustard, you need to have your eyes dilated and carefully examined by a professional.
Diabetic eye disease includes cataract, diabetic retinopathy and glaucoma. Cataract and glaucoma also affect people who do not have diabetes. A common type of diabetic retinopathy is non-proliferative diabetic retinopathy. With this problem, small blood vessels leak causing the retina to swell. This is macular edema. The result is blurred vision. It may occur in only a part of the vision as noted in the image.
If you have diabetes PLEASE get an eye exam yearly!!
Diabetic Kidney Disease
 Diabetic nephropathy, (kidney disease from diabetes) is the most common cause of kidney failure and the need for dialysis. About 20-40% of patients with diabetes will end up with kidney disease. Elevated blood sugar causes damage to the delicate filtering part of the kidneys (glomeruli). This damage is painless and can be gradually getting worse over several years without symptoms. The most common early sign of diabetic kidney disease is protein in the urine. Occasionally there is blood in the urine. Medical professionals commonly check urine for protein looking for early signs of diabetic kidney damage. An ordinary urinalysis may not show the problem. The test to screen for early protein in the urine is called albumin/creatinine ratio. This screening test should be done at least annually in patients with diabetes. Diabetic nephropathy occurs in all forms of diabetes. Elevated blood pressure is an additional insult to the filtering system of the kidney. It may be even more important than blood sugar.
Diabetic nephropathy, (kidney disease from diabetes) is the most common cause of kidney failure and the need for dialysis. About 20-40% of patients with diabetes will end up with kidney disease. Elevated blood sugar causes damage to the delicate filtering part of the kidneys (glomeruli). This damage is painless and can be gradually getting worse over several years without symptoms. The most common early sign of diabetic kidney disease is protein in the urine. Occasionally there is blood in the urine. Medical professionals commonly check urine for protein looking for early signs of diabetic kidney damage. An ordinary urinalysis may not show the problem. The test to screen for early protein in the urine is called albumin/creatinine ratio. This screening test should be done at least annually in patients with diabetes. Diabetic nephropathy occurs in all forms of diabetes. Elevated blood pressure is an additional insult to the filtering system of the kidney. It may be even more important than blood sugar.
What to do?.
Control blood sugar on a day to day basis.
Ensure that your A1c is at the target set for you by your medical professional.
Control your blood pressure.
Avoid diet sodas. Do not smoke.
Take your medication faithfully.
Your medical professional may prescribe specific high blood pressure medicines that help prevent additional damage to the kidneys. These include the ACE inhibitors and the ARB’s. Once the process of diabetic nephropathy has started, you may be prescribed a low protein diet to reduce the workload of the kidneys.
The Dawn Phenomenon
This early morning rise in blood sugar is the effect of increased hormones overnight. We like to say, “this is your body’s way of getting you ready for the day”. The main 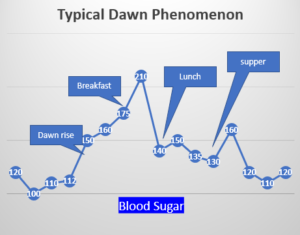 source of energy is glucose (sugar) you’re going to need increased energy as you get up and start moving around. The increase in hormones is a part of the biological clock. These can be measured and are almost invariably found to be higher in the morning. Hormones involved in this process include adrenaline, cortisol, growth hormone, cortisol and glucagon. For this reason, swing shift work can make diabetes control extremely difficult. When I was in Southeast Wisconsin (highly unionized) we could get an employer to avoid swing shifts in our diabetic patients. Not so in South Carolina!
source of energy is glucose (sugar) you’re going to need increased energy as you get up and start moving around. The increase in hormones is a part of the biological clock. These can be measured and are almost invariably found to be higher in the morning. Hormones involved in this process include adrenaline, cortisol, growth hormone, cortisol and glucagon. For this reason, swing shift work can make diabetes control extremely difficult. When I was in Southeast Wisconsin (highly unionized) we could get an employer to avoid swing shifts in our diabetic patients. Not so in South Carolina!
What to do?
This can be difficult, take no action until you have consulted your health care professional. One cannot turn hormone release off. Many feel it is necessary to have a nighttime snack to avoid overnight low blood sugar (hypoglycemia). This may not be true with the slow (long-acting) insulins such as Lantus, Levemir, Basaglar, Toujeo, Tresiba. Nevertheless, overnight LOW blood sugar can be dangerous and should be avoided.
Here are some strategies.
- Get your overall, average blood sugar in control. Try to meet your target A1c set by your health care professional. This reduces the effect of the dawn phenomenon.
- Check blood sugar overnight (generally between 2 and 3 AM). If sugar is very high, you might be able to avoid or at least limit the nighttime snack. If you skip this snack, check again several times overnight to see if you are having an unrecognized low sugar.
3. Limit carbohydrates and fat in the evening meal. - Do something active after the evening meal such as taking a walk.
Vitamin D
It is a good idea to have a recommended vitamin D level. In addition to advantages for bone health, vitamin D appears to improve immunity and may and may reduce the fatal effects of COVID-19.
Evidence for vitamin D and COVID-19
1.“Vitamin D deficiency may partly explain the geographic variations case fatality rate of COVID-19, implying that supplementation with vitamin D MAY reduce the mortality from this pandemic.” Med Drug Discov. 2020 Apr 29 : 100041 However, high-dose vitamin D does not help and may be harmful.
2.“Researchers analyzed patient data from 10 countries. The team found a correlation between low vitamin D levels and hyperactive immune systems. Vitamin D strengths innate immunity and prevents overactive immune responses. The finding could explain several mysteries, including why children are unlikely to die from COVID-19.” From Science Daily.com and Northwestern University.
3.“Vitamin D levels are severely low in the aging population especially in Spain, Italy and Switzerland. This is also the most vulnerable group of population for COVID-19.” www.researchsquare.com
Vitamin D supplementation is confusing because there are differing recommendations. The FDA recommends a minimum intake 400 IU daily. Other groups including the Endocrine Society recommends as much as 1000-2000 IU. Vitamin D is essential for calcium and phosphorus regulation, bone health. Low vitamin D levels have been associated with high blood pressure immune function, nervous system function, cancer, diabetes, thyroid disease and others.
Vitamin D has not been established as the cause of many of these, they are simply found together. If you and I showed up at the local Walmart at the same time, it does not mean that one of us caused the other to be there. Nevertheless, it is prudent to take some vitamin D, especially if sun exposure is limited
Too much vitamin D elevates blood calcium resulting in several problems including nausea, vomiting, weakness and kidney stones. How much is too much? Vitamin D toxicity has been shown in cases taking as much as 60,000 IU daily.
Pain Pain Pain
In the quest to relieve pain, remember, what you put on you is less likely to cause problems than what to put in you. For this reason, I have become a fan of products containing Arnica Montana. No one knows how this stuff works but it has been shown to reduce pain in osteoarthritis and to reduce bruising. There are several homeopathic products to be taken by mouth but it’s a good idea to avoid these. The creams/gels have few side effects but should not be placed in open cuts, wounds or broken skin. Don’t use during pregnancy.
There are several Arnica Montana products available in creams, gels, as a roll on etc.
They must be rubbed into the skin. The effect is not immediate. About 60% of people we recommended it to indicate some pain relief. I use it for my painful shoulder, back and fingers. It is effective enough for me to get back to sleep after being awakened by pain.
Features
- Available without prescription at most pharmacies.
- Few if any side effects applied to intact skin
- No odor
- Starts to work in about 5 minutes
- It boosts the effect of other pain medicines such as Tylenol (acetaminophen), ibuprofen, Advil etc.
Glucose Toxicity
Are you taking tons of insulin and/or pills but still can’t seem to control your blood sugar? You may have glucose toxicity. In glucose toxicity, the body does not respond well to insulin. The response is poor whether the insulin is from the pancreas or injected/inhaled. It comes from prolonged exposure to high blood sugars. If you improve insulin sensitivity, insulin works better. Improved insulin sensitivity ⇒ reduced glucose toxicity. If taking insulin and you increase sensitivity, you may risk low blood sugars. Do not approach this unless approved by your healthcare professional.
Items to help you improve insulin sensitivity
- Lose weight. The more of you there is, the more insulin you need.
- Exercise more. Exercise increases sugar uptake in tissues and increases sensitivity to insulin
- Reduce stress. Stress causes an increase in hormones that raise blood sugar thereby increasing the need for insulin.
- Eat more high-fiber foods. Fiber slows sugar absorption from your G.I. tract and gives you a full feeling, so you may eat less.
- Improve diabetes control. Talk to your health care professional about adding additional medications to improve control. the better the control, the better the insulin sensitivity.
- Add nasty tasting food to your diet. Evidence in this area is spotty and contradictory. There are reports that Apple cider vinegar, pumpkin, pumpkin seeds, okra water (and others) improve insulin sensitivity. It may be that eating more nasty tasting foods reduces the amount of good tasting stuff that increase blood sugar 😊.
Dehydration
Dehydration is defined as a harmful loss of body water. It is especially dangerous in ALL types of diabetes.
dangerous in ALL types of diabetes.
Ordinary fluid loss
- Normal body functions cause loss of 20 – 30 oz fluid daily (insensible fluid loss).
- Skin, the natural radiator, attempts to reduce body heat by producing sweat which cools as it evaporates.
- The kidneys attempt to eliminate high blood sugar by pulling water and sugar into urine.
Abnormal fluid loss.
- Problems with the stomach and intestines causing vomiting or diarrhea.
- Excessive heat exposure.
- Excessive exercise.
- Kidney disease.
- Diuretics (water pills).
- Diabetes mellitus.
- Diabetes insipidus.
- Some diabetes medicines. See List
Some signs of dehydration
- Thirst
- Dizziness
- Rapid heart rate.
- Rapid breathing.
- Decreased pee.
- Very dark urine.
How to avoid dehydration
- When the weather is hot, be aware of how you feel.
- Limit strenuous exercise when the weather is hot.
- Drink water regularly.
- Avoid caffeine e.g. coffee, tea, caffeinated soft drinks.
- Avoid or limit drinks with alcohol.
Sport drinks like Gatorade. I have always been fascinated by the Gatorade story. Southern football teams, especially the University of Florida in the 1960s, recruited players from all over. Pre-season practice occurred during the hottest months of the year. These kids, unaccustomed to the heat were passing out from dehydration and having muscle cramps when water was used for dehydration. The coaches requested help from the University of Florida College of Medicine. It is rumored that the scientists gathered sweat towels from the football team, rung them out and analyzed the content. A cocktail was produced based on the chemical content of the team’s sweat. The result was a mixture of water, sodium, sugar, potassium, phosphate and lemon juice. Experiments with the mixture were successful. The football team credited Gatorade in Florida’s first Orange Bowl will win over Georgia Tech in 1967. Steve Spurrier was the quarterback in that game. Last year, Gatorade sales were reported at ~$5 billion.
Some sports drinks contain carbs. Under ordinary circumstances people with diabetes don’t need extra sugar in sports drinks. However, a judicious amount of carbohydrate is needed to avoid the production of ketones if there is adequate insulin (natural or injected) to handle it.
Carbohydrate content of some Gatorade products (12 oz).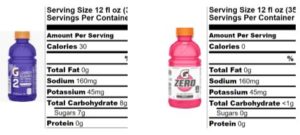
- G Gatorade contains 34 g carbohydrate.
- G2 Gatorade contains 8 g of carbohydrate.
- G Zero Gatorade contains less than 1 g. carbohydrate.
Note: when reading labels, always look at the total carbohydrate content, NOT the sugar content. Non-sugar carbohydrate will still affect your blood sugar.
SGLT2 drugs.
These products work by increasing glucose in the urine thereby decreasing blood glucose (sugar). To accomplish that, it is necessary to pull water from the body. Dehydration is a risk.
Below is a list of these products.
- canagliflozin (Invokana)
- dapagliflozin (Farxiga)
- empagliflozin (Jardiance)
- empagliflozin/linagliptin (Glyxambi)
- empagliflozin/metformin (Synjardy)
- dapagliflozin/metformin (Xigduo XR)
- Qtern (dapagliflozin and Saxagliptin)
Fried chicken and blood sugar
Food fried in oil (boiled in oil) results in elevated blood free fatty acids.  This increases insulin resistance (decreases the effect of insulin whether natural, injected or inhaled).
This increases insulin resistance (decreases the effect of insulin whether natural, injected or inhaled).
My challenge to folks with type 2 diabetes who love fried foods. Don’t do this unless approved by your healthcare professional.
- Check blood sugar.
- Eat 2 pieces of fried chicken – eat nothing else.
- Check blood sugar at 1 and 2 hours.
Wow!
Is it okay for people with diabetes to eat fried chicken? Of course. Help yourself, just don’t take too much.
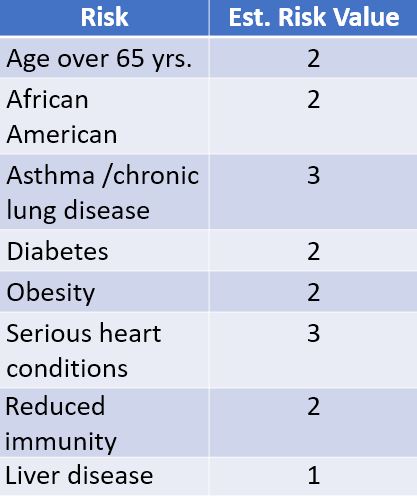
Welcome to summer. About this time every year, A1c levels of our patients are anywhere from 1 – 2 percentage points higher than the rest of the year (except Thanksgiving/Christmas). We think it’s because of the ready availability of those wonderful melons and fruits.
A piece of bread contains about 15 g of carb. ![]() A tiny slice of watermelon like this contains about 27 g of carb. But who eats it like that? A vigorous slice of watermelon is at least 3 -4 times that much, up around 100gm that’s in the range for 3 glazed Donuts. Guess what that will do to your blood sugar
A tiny slice of watermelon like this contains about 27 g of carb. But who eats it like that? A vigorous slice of watermelon is at least 3 -4 times that much, up around 100gm that’s in the range for 3 glazed Donuts. Guess what that will do to your blood sugar
Food in relation to blood sugar is not so much what you eat but how much you swallow!!. A reasonable amount will generally not have a great effect but follow an unrestrained appetite–there is trouble in the air.