You may now see your glucose information on almost any smartwatch (Apple Watch, android Samsung, Garmin etc.) The app is called Gluroo: Diabetes Log Tracker. PROs: 1. High and low glucose alarms are available on your wrist. 2. It connects directly to the Decom Clarity or Libre View apps on your phone. 3. It is free.
CONs: 1. The associated watch face is ugly. 2. The legal agreement states it will sell your personal information, including credit card information. At least they are upfront about it, I don’t think they can extract credit card information if you don’t give it to them. 3. If you change the watch face to something more presentable you will have to reopen the app on the phone to get updated glucose information on your watch. 4. Setting it up is not easy, you may want to get help from a teen-ager. 5. Not FDA approved. Click here for details.

Inserting Libre 3
Inserting Dexcom G6
Inserting Libre 2
Inserting Dexcom G7
The newest no finger stick gadget available for estimating glucose is the Dexcom G7. So how does it compare to the Libre3?

Dexcom G7 and Freestyle Libre3 are both continuous glucose monitoring (CGM) systems used to monitor their blood glucose levels throughout the day. While both systems have similarities, there are also some differences to consider.
Here are some key differences:
- Sensor Wear Time: The Dexcom G7 sensor is designed to be worn for up to 14 days, while the Freestyle Libre3 sensor can be worn for up to 14 days.
- Sensor Placement: The Dexcom G7 sensor is inserted under the skin using an applicator, typically on the abdomen or upper buttock, while the Freestyle Libre3 sensor is applied to the back of the upper arm with a small applicator.
- Real-Time Monitoring: The Dexcom G7 provides real-time glucose readings and alerts to a compatible device such as a smartphone or smartwatch, while the Freestyle Libre3 requires a handheld reader or smartphone to scan the sensor to get a glucose reading.
- Cost: The cost of both systems may vary depending on insurance coverage and location. In general, the Dexcom G7 may be more expensive than the Freestyle Libre3.
- Accuracy: Both systems have been shown to be accurate in clinical studies, but individual experiences may vary.
Ultimately, the choice between Dexcom G7 and Freestyle Libre3 will depend on personal preferences, lifestyle, and individual healthcare needs.
Can Tylenol or other forms of acetaminophen cause false blood sugar readings on sensor?

Medtronic Guardian and 670g systems Yes*
- Taking medications with acetaminophen, including, but not limited to Tylenol, fever reducers, or cold medicine, while wearing the sensor may falsely raise your sensor glucose readings. Avoid taking medications with acetaminophen while in Auto Mode with Medtronic 670g.
Dexcom CGM systems (G4/G5) Yes, G6 No*
- Systems (G4/G5), acetaminophen could affect your sensor readings, making them look higher than they really were. However, with the G6, you can take a standard or maximum acetaminophen dose of 1 gram (1,000mg) every 6 hours and still use the G6 readings to make treatment decisions.
Abbott FreeStyle Libre No, but vitamin C may affect readings. *
- Taking ascorbic acid (vitamin C) while wearing the Sensor may falsely raise Sensor glucose readings. Taking salicylic acid (used in some pain relievers such as aspirin and some skin care products) may slightly lower Sensor glucose readings.
*From manufacturers user guides
What about the effect of acetaminophen (Tylenol ®) on fingerstick glucose meter tests? There is not much to worry about if a person has no liver disease and follows dose guidelines. Meters using the glucose oxidase method are more likely to be interfered with by substances such as acetaminophen, vitamin C, and dopamine. Some meters using this method include AgaMatrix, Novo Max, OneTouch Ultra2 (but not Verio) and ReliOn Prime.
Acetaminophen safety. The big issue is taking too much can cause liver damage, sometimes serious enough to require liver transplantation or death.
To be sure that you take acetaminophen safely, you should
- not take more than one product that contains acetaminophen at a time. Read the labels of all prescription and nonprescription medications to see if they contain acetaminophen. Be aware that abbreviations such as APAP, AC, Acetaminophen, Acetaminoph, Acetaminop, Acetamin, or Acetam. may be written on the label in place of the word acetaminophen. Ask your doctor or pharmacist if you don’t know if a medication contains acetaminophen.
- take acetaminophen exactly as directed on the prescription or package label. Do not take more acetaminophen or take it more often than directed, even if you still have fever or pain. Ask your doctor or pharmacist if you do not know how much medication to take or how often to take your medication. Call your doctor if you still have pain or fever after taking your medication as directed.
- be aware that you should not take more than 4000 mg of acetaminophen per day. If you need to take more than one product that contains acetaminophen, it may be difficult for you to calculate the total amount of acetaminophen you are taking. Ask your doctor or pharmacist to help you.
- tell your doctor if you have or have ever had liver disease.
- not take acetaminophen if you drink three or more alcoholic drinks every day. Talk to your doctor about the safe use of alcohol while you are taking acetaminophen.
- stop taking your medication and call your doctor right away if you think you have taken too much acetaminophen, even if you feel well.
Talk to your pharmacist or doctor if you have questions about the safe use of acetaminophen or acetaminophen-containing products. Source: NIH MedlinePlus
Abbott Freestyle Libre™
LibreLink® app allows use of phone as reader
Abbott FreeStyle Libre is now available without insurance for about $116/mo. If you are testing 3-4 times daily it could be cost effective to avoid fingersticks.
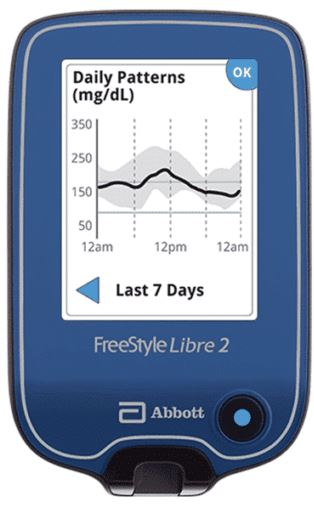


As of November 14, 2018, available for iOS in US, Android expected soon
PROs
- Applied to back of arm with self-contained device.
- Fingerstick calibrations not required (see exceptions below).
- Good insurance coverage (including some part D Medicare plans with restrictions).
- Sensor lifespan 14 days.
- Readings availabe in one hour after sensor start
- Reader can be used as a fingerstick meter
- Phone app reader available for iOS now. Anroid now in Europe expected here soon.
CONs
- No alarms and no predictive alerts.
- Vitamin C and salicylic acid interference.
- Will not communicate with insulin pump (See Libre transmitters below).
Details
- The Libre system consists of a patch sensor and a reader/meter.
- Upon insertion, a tiny sensor is placed beneath the skin.
- The sensor must be replaced in 14 days (10 days on the original system).
- The reader must be placed near the sensor to obtain glucose information.
- The reader does not provide alerts or warnings. (See Libre transmitters below).
- Arrows are provided on the reader to indicate rapidly increasing or decreasing glucose.
- The reader screen will indicate the need for a fingerstick blood glucose when readings are less than 70 or greater than 500 mg/dl.
A finger prick test using a blood glucose meter is required during times of rapidly changing glucose levels when interstitial fluid glucose levels may not accurately reflect blood glucose levels or if hypoglycemia or impending hypoglycemia is reported by the Sensor or when symptoms do not match the Sensor readings.
- As with any subcutaneous glucose sensor, there may be a significant difference between blood glucose and the sensor reading. Sensor data can be as much as 15 – 20 minutes behind the fingerstick when blood glucose is moving rapidly e.g. after eating.
- Taking ascorbic acid (vitamin C) while wearing the Sensor may falsely raise Sensor glucose readings. Taking salicylic acid (used in some pain relievers such as aspirin and some skin care products) may slightly lower Sensor glucose readings.
- The sensor is operational while wet but should not be taken below 3 feet of water and submerged for more than 30 minutes
PRICE: the reader and a month of sensors can be purchased for approximately $200 without insurance. Thereafter, retail price ranges from $120 – $130 per month. This information derived from my personal purchases in Orangeburg South Carolina.
Dexcom G6™

PROs
- High level of accuracy and dependability.
- 10 day sensor duration.
- Fingerstick calibration nonrequired.
- FDA approved treatment decisions (e.g. insulin administration) without confirming fingersticks
- Transmits glucose data and alerts to insulin pump
- Glucose information transmitted to phone/watch.
- High and low glucose alerts on sensor and phone/watch.
- Predictive alerts.
CONs
- Transmitter life limited to 3 months. Earlier less sophisticated versions (G4) lasted 6 months.
- As with any subcutaneous glucose sensor, blood glucose and sensor readings may differ. The sensor reading might lag as much as 15 – 20 minutes behind the fingerstick.
- Price
DEXCOM
The Dexcom G6 CGM is FDA-permitted to make diabetes treatment decisions without confirmatory fingersticks or calibration. However, if glucose alerts and readings from the G6 do not match symptoms or expectations, one must use a blood glucose meter to make diabetes treatment decisions.
Trend lines show where glucose levels are headed and how fast they’re getting there, so you can take action.
It appears smart phone/watch compatibility is limited to specific devices. Reviews on Google Play are very negative. A list of compatible devices including android, iPhones and iPads (US) can be found here.
COST: Transmitter $286. Three sensors with inserters $379.10
The Eversense™ Long-Term CGM System
Here’s what I know about the Eversense system so far.
PROs
- Implantable sensor lasts up to 90 days.
- Glucose information transmitted to phone.
- High and low glucose alerts on sensor and phone.
- Predictive alerts.
- The sensor remains in place even if the transmitter is removed or knocked off.
CONs
- Old sensor must be removed and a new one inserted under the skin by physician every 90 days.
- Transmitter must be removed and charged daily; then replaced with new adhesive.
- Fingerstick blood glucose calibration required twice daily.
- As with any subcutaneous glucose sensor, there may be a significant difference between blood glucose and the sensor reading. This can be as much as 15 – 20 minutes behind the fingerstick.
- Price
Details
- The sensor must be implanted under the skin by a physician.
- Sensor size 5mm (0.73 in) X 3.5mm (0.15 in)
- The sensor provides glucose monitoring for “up to 3 months”.
- Fingerstick blood glucose calibration required twice daily.
- The transmitter fits over the spot where the sensor has been inserted.
- The transmitter is removable and rechargeable.
- Glucose data is transmitted by Bluetooth to a telephone (android or IOS).
- Transmitter provides vibration alerts with low or high glucose even if the telephone is not nearby.
- Transmitter is water resistant submerged in 3 feet up to 30 minutes.
- The transmitter must be charged daily and does not receive data while charging.
- Charge time for the transmitter is indicated as 15 minutes.
- A fingerstick blood glucose must be done before making a treatment decision such as taking insulin.
- The sensor has a silicone ring that contains a small amount of an anti-inflammatory drug (dexamethasone acetate).
- Sensor operation only occurs between temperatures of 81 – 104.0°F
- As with any subcutaneous glucose sensor, there may be a significant difference between blood glucose and the sensor reading. Sensor data can be as much as 15 – 20 minutes behind the fingerstick when blood glucose is moving rapidly e.g. after eating.
COST: Insurance coverage unknown, cost anticipated at about $240 monthly. Insertion/removal device is advertised on the Internet at $1300+.
