Low thyroid? It could be Hashimoto's thyroiditis
- Hashimoto’s thyroiditis, also known as Hashimoto’s disease, is an autoimmune disorder that affects the thyroid gland.
- The thyroid gland produces hormones that play a crucial role in regulating your metabolism and overall energy levels.
- In Hashimoto’s thyroiditis, your immune system mistakenly identifies the thyroid gland as a threat and starts attacking it. This attack leads to inflammation and damage to the thyroid tissue. Over time, this can interfere with the thyroid’s ability to produce enough hormones, leading to an underactive thyroid or hypothyroidism.
- The exact cause of Hashimoto’s thyroiditis is not fully understood, but it is believed to involve a combination of genetic factors and environmental triggers. Some potential triggers may include viral infections, hormonal imbalances, or excessive iodine intake.
- Hashimoto’s thyroiditis predominantly affects women, and it often develops gradually over several years. In the early stages, one may not experience any noticeable symptoms. As the condition progresses and your thyroid function declines, you may start to experience various symptoms such as fatigue, weight gain, sensitivity to cold, constipation, dry skin, and hair loss. Some individuals may also develop a goiter, which is an enlargement of the thyroid gland.
- Diagnosing Hashimoto’s thyroiditis typically involves a combination of blood tests that measure thyroid hormone levels and detect the presence of specific antibodies associated with the condition. Treatment usually involves taking synthetic thyroid hormones to replace the hormones that your thyroid gland is not producing adequately.
- While Hashimoto’s thyroiditis is a chronic condition, with proper management and medication, most people can live a normal and healthy life. Regular monitoring of thyroid hormone levels and ongoing medical care are necessary to ensure that the thyroid function is adequately regulated.

Biotin
High doses of biotin have been shown to interfere with thyroid function tests. This supplement, a form of vitamin B has also been called vitamin H. The most common moniker is vitamin B7. Biotin is promoted as a supplement for thin hair, brittle nails and fatigue. A recommended daily amount for biotin is approximately 30 micro-grams, it is widely available in doses from 5,000 to 10,000 micro-grams. A bottle of 120 capsules of biotin ($19.99 Amazon) is claimed as an important component of enzymes that breakdown fats and carbohydrates, improves hair health, skin and nails.
Natural sources of Biotin (Wikipedia)
Biotin can cause a falsely low TSH and high free T4 and free T3. This combination could cause a wrong diagnosis of hyperthyroidism and even treatment with anti-thyroid medication. On the other hand, a person taking levothyroxine (e.g. Synthroid) for hypothyroidism could have an unnecessary and possibly dangerous decrease in the dose needed for thyroid replacement.
Taking 5000 micro-grams or more of Biotin can interfere with thyroid function tests. Patients taking biotin should hold the supplement for two days prior to thyroid function tests and longer if they are taking more than 1000 micro-grams a day according to UpToDate®
Your Thyroid and Radioactivity
What do nuclear power plants and the Savannah River site have to do with your thyroid? Not anything if everything goes well. The thyroid gland traps any iodi ne absorbed into the human body. If that iodine is radioactive, there is increased risk of thyroid cancer, especially in children. Radioiodine is formed close to us at the Savannah River site and the Alvin W. Vogtle Electric Generating Plant (about 10 miles away in GA) as a byproduct of nuclear reactive operations. Radioisotopes of iodine have been released to the atmosphere from the Savannah River site since 1955 according to a 1990 report from the US Department of Energy.
ne absorbed into the human body. If that iodine is radioactive, there is increased risk of thyroid cancer, especially in children. Radioiodine is formed close to us at the Savannah River site and the Alvin W. Vogtle Electric Generating Plant (about 10 miles away in GA) as a byproduct of nuclear reactive operations. Radioisotopes of iodine have been released to the atmosphere from the Savannah River site since 1955 according to a 1990 report from the US Department of Energy.
A Savannah River Site report indicates no radioactive gas release in 2017, the latest I could find. There have been releases over the past 10 years however. See chart. There is an interesting article from the Charleston Post and Courier here.
What to do?
Ensure enough iodine intake to avoid deficiency (increases the risk of a nodular goiter). The World Health Organization recommends 150 mcg daily for adults. One teaspoon of iodized salt contains approximately 400 μg iodine. Fish, shrimp, other seafood and dairy products are generally rich in iodine.
If there is a nuclear incident, follow medical advice which will probably include taking potassium iodide (KI). The Nuclear Regulatory Commission now recommends 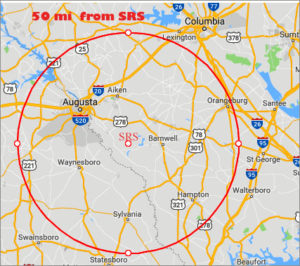 evacuation if living within 50 miles of a nuclear event. If a person has or is expected to have radiation exposure, potassium iodide (KI) is protective. It protects by saturating the gland with iodine thereby preventing absorption of the radioactive product. KI does not prevent radioactive iodine from being absorbed and cannot reverse effects caused by it once the thyroid is damaged. It only protects the thyroid, not other parts of the body.
evacuation if living within 50 miles of a nuclear event. If a person has or is expected to have radiation exposure, potassium iodide (KI) is protective. It protects by saturating the gland with iodine thereby preventing absorption of the radioactive product. KI does not prevent radioactive iodine from being absorbed and cannot reverse effects caused by it once the thyroid is damaged. It only protects the thyroid, not other parts of the body.
Iodized table salt and foods do not contain enough iodine to block radioactive iodine. Table salt is not recommended as a substitute for KI. Potassium iodine should only be taken upon recommendation of health officials or medical practitioners according to the CDC. Side effects of KI (potassium iodide) include fever, joint pain, feeling anxious as well as allergic reactions that include rash, hives, wheezing and shortness of breath.
Thyroid Nodules
A thyroid nodule is an abnormal growth within the thyroid gland that creates a lump. A few thyroid nodules contain cancer. As with all cancers, the earlier the detection, the better the outcome.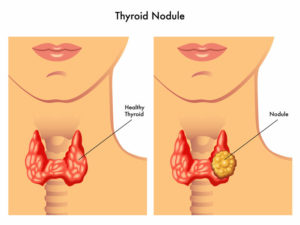
Thyroid nodules are often discovered during a routine physical examination or on tests as ultrasound, CAT scan or MRI done for non-thyroid reasons. Occasionally the patient will notice a lump in the neck while looking the mirror. There was a case in which a viewer noticed a lump on the neck of a TV personality, notified the person and it turned out thyroid cancer which was treated promptly.
Most thyroid nodules have no symptoms. The patient often does not know it is there. There may be pain in the neck or difficulty swallowing if the gland is large. A tickle in the neck occurs occasionally.
The cause of a thyroid nodule is generally not known. By age 60, half in the people in the world have at least one thyroid nodule. Over 90% of these are not cancerous. Hashimoto’s thyroiditis is a source of nodules. Iodine deficiency has been associated with nodules, but this is not generally found in the US because of ready sources of iodine including iodized salt. Just as there is an awful lot of coffee in Brazil, there is an awful lot of salt and hypertension in the US.
If a nodule is discovered, the first tests are generally thyroid blood tests for inflammation, over or under activity of the gland. These are often normal. A thyroid ultrasound is likely the next test. The ultrasound can detect if there is a suspicious nature of the nodule needing to additional tests. This might include a scan of the thyroid after a small dose of radioiodine to determine if the nodule is functioning. If there is a suspicion of possible malignancy in the gland, a biopsy may be requested. This is called an FNA (fine-needle aspiration). In this test, a small amount of tissue is drawn from the nodule with a tiny needle and submitted for pathologic evaluation. Most often, there is no cancer. If no evidence of cancer, the recommendation is for periodic ultrasound follow-up to ensure the nodule has not changed or become more suspicious.
 Got brain fog, tired. Can it be your thyroid? How about a thyroid supplement?
Got brain fog, tired. Can it be your thyroid? How about a thyroid supplement?
More than 50% of Americans say they are tired. Fatigue is said to cause 7 million medical office visits annually. Fatigue is a frequent symptom of thyroid disease therefore some focus on it as the cause of recurrent tiredness. Obviously, there are a plethora of conditions that can make one tired. Disorders of the thyroid are among these. Before jumping to supplements, consult your licensed medical professional. Click here for common causes of chronic fatigue.
Supplements. Marketers of “Thyroid Supplements” claim healthy weight and energy management plus treatment for hypothyroidism. Some are mixed in with probiotics and most contain selenium. Worst of all some contain THYROID HORMONE!! Supplements are not subject to the level of scrutiny as prescription items. The FDA indicates “Manufacturers and distributors of dietary supplements and dietary ingredients are prohibited from marketing products that are adulterated or misbranded. That means that these firms are responsible for evaluating the safety and labeling of their products before marketing to ensure that they meet all the requirements of DSHEA and FDA regulations” – emphasis added. The agency further states “The U.S. Food and Drug Administration (FDA) does not have the authority to review dietary supplement products for safety and effectiveness before they are marketed.”
Common symptoms of altered thyroid function.
Under-active thyroid conditions (hypothyroidism).
Cold intolerance, weight gain, constipation, dry skin, fatigue.
Overactive thyroid conditions (hyperthyroidism)
Heat intolerance, weight loss, diarrhea, dry skin, fatigue.
One in eight Americans will have some thyroid issues in their lifetime, according the American Thyroid Association. The group also indicates 60 % of these will not be aware of it.
Thyroid hormones are secreted by the thyroid gland, a butterfly shaped organ at the front of the neck. They are essential for brain and body development in infants and for metabolic activity in adults. We like to describe thyroid hormone as the accelerator of the body. Too little and everything slows. Too much and everything goes too fast.
The thyroid requires iodine to produce its hormones. The gland doesn’t require much, 5gm is said to meet the life-time needs of an individual. Insufficient iodine intake causes the thyroid to enlarge (develops a goiter) as it tries to keep up with demand for thyroid hormone. Iodine deficiency was common in parts of America before the introduction of iodized salt. It is not much of a problem now because we certainly get enough salt. NOTE: some sea salts don’t contain iodine. It is difficult to know if prepared or canned food processors use iodized salt. The Harvard Health letter indicates most food companies don’t use iodized salt. You can reduce salt intake (nearly all prepared foods contain salt) without affecting iodine intake because common sources of iodine (excluding iodized salt) include: eggs cheese, cow’s milk and milk products, shellfish, soy milk and soy sauce.
Some conditions causing fatigue
| Condition | Symptoms |
| Congestive Heart Failure | Shortness of breath walking or lying flat, swelling of legs. |
| Obstructive Lung disease (COPD) | Shortness of breath, chronic cough, sputum. |
| Sleep apnea | Snoring, interrupted breathing during sleep. |
| Hypothyroidism (underactive thyroid) | Cold intolerance, weight gain, constipation, dry skin. |
| Hyperthyroidism (overactive thyroid) | Heat intolerance, weight loss, diarrhea, moist skin, palpitations. |
| Uncontrolled diabetes | Hunger, thirst, frequent urination. |
| Chronic kidney disease | Nausea/vomiting, mental status changes, decreased urine. |
| Chronic liver disease | Abdominal distention, gastrointestinal bleeding |
| Anemia | Dizziness, weakness, palpitations, shortness of breath |
| Mononucleosis syndrome | Fever, sore throat, tender lymph nodes |
| HIV infection | Weight loss, variable localized complaints |
| Polymyalgia rheumatica | Aching/morning stiffness of shoulders, neck, and hips |
| Fibromyalgia | Chronic widespread muscle pain |
| Depression | Sad mood, anhedonia, altered sleep, cognitive dysfunction |
| Anxiety disorder | Generalized nervousness, panic attacks, phobias. |
| Medication toxicity/Substance abuse* | Variable |
*Medications frequently associated with fatigue include: Benzodiazepines, antidepressants, muscle relaxants, first-generation antihistamines, beta-blockers, opioids, alcohol, marijuana, opioids, cocaine/other stimulants. Reference: UpToDate
Thyroid Awareness
Thyroid awareness
Have a diagnosis of thyroid problems? You’re in good company. In a room of 8 women, at least one will have some form of a thyroid problem in her lifetime. Men also have thyroid problems, but women are more likely, 5 to 8 times more likely to develop a thyroid issue. According to the American thyroid Association, up to 60% of people with thyroid disease are not aware of it.
The thyroid gland sits at the base of the neck. It secretes a hormone that regulates metabolism.That hormone affects every part of the body. Symptoms of thyroid disease may be nonspecific and remain undiagnosed. The thyroid is like the accelerator for your body. Too much and things go too fast, too little and things slow down. Thyroid hormone replacement has been used to accelerate weight loss, IT DOESN’T WORK!
Common symptoms of an underactive thyroid: HYPOthyroidism
- Weight gain.
- Slow heart rate.
- Sensitivity to cold.
- Thinning hair.
- Constipation.
Common symptoms of an overactive thyroid: HYPERthyroidism
- Palpitations, increased heart rate.
- Weight loss.
- Increased sweating, heat intolerance.
- Nervousness and anxiety.
- Sleep disorder.
- Frequent bowel movements
Hashimoto’s thyroiditis is the most common cause of an underactive thyroid gland (hypothyroidism). It is an autoimmune problem in which the body’s immune system attacks the thyroid gland. In rheumatoid arthritis the body’s immune system attacks the joints; in Hashimoto’s thyroiditis it pounces upon the thyroid gland. The inflammation causes the gland to extrude stored thyroid hormone. This results in symptoms of an overactive thyroid. Over time, the inflammation restricts the gland’s ability to make thyroid hormone, the person now has hypothyroidism.
Hashimoto’s thyroiditis does not have specific symptoms. It is most often diagnosed when a person presents with symptoms of hypothyroidism. In early stages symptoms of hyperthyroidism may be present. This form of thyroid inflammation can be diagnosed with a simple blood test. We see several patients with no symptoms but mildly abnormal thyroid function tests. If a diagnosis of Hashimoto’s thyroiditis is made, treatment is symptomatic, in other words treat the symptoms of an overactive or underactive thyroid.
Generic vs branded
 We are rarely able to get insurance to pay for non-generic levothyroxine. Here’s why: The retail price for Synthroid® oral tablets 25 mcg (0.025 mg) is around $96 for 90 tablets, depending on the pharmacy you visit. Drugs.com
We are rarely able to get insurance to pay for non-generic levothyroxine. Here’s why: The retail price for Synthroid® oral tablets 25 mcg (0.025 mg) is around $96 for 90 tablets, depending on the pharmacy you visit. Drugs.com
The retail price of generic levothyroxine (30 tablets) varies from $4.00 (Walmart) to $9:61(Walgreens). GoodRx.com
Are generic drugs equal to “branded” ones? Levothyroxine has a narrow therapeutic window meaning the range between a proper dose and a toxic one is narrow. Undertreatment or over treatment of a thyroid problem can lead to numerous problems, including heart conditions. Am I getting the proper amount of levothyroxine if it’s generic?
FDA: “all levothyroxine sodium products approved for use in humans will meet a 95% to 105% potency specification throughout their labeled shelf-lives.“
If you are taking 100μg of levothyroxine, an FDA approved generic tablet could be at 95μg but if the pharmacy switches manufacturer, you could be getting the equivalent of 105μg. That said, we found a study indicating: “To date (2005), no generic product accepted as equivalent using FDA Guidance has been shown to result in a safety and efficacy profile different from its brand counterpart.” The AAPS Journal, March 2005, Volume 7, Issue 1, pp E47–E53.
A little change in levothyroxine potency can have major consequences. Getting too much or too little could result in return of symptoms, osteoporosis, atrial fibrillation,worsening of coronary heart disease and/or congestive heart failure, early delivery in pregnancy, and rising cholesterol. Those especially prone to improper doses of levothyroxine include the elderly, pregnant women and their developing fetuses, and those with thyroid cancer. The current recommendation by the FDA for patients switching between levothyroxine products is to have repeat thyroid function testing to allow for dose change. We test all patients on thyroid replacement at least annually. If one must take generic levothyroxine, check the label on bottle for the manufacturer (e.g Forest Laboratories, Mylan) if it’s different from the one before, request a repeat set of thyroid function tests.
Notes on levothyroxine:
- Some foods: soybean flour, cottonseed meal, milk, walnuts, dietary fiber and grapefruit juice may reduce absorption of levothyroxine.
- Take levothyroxine as a single dose on an empty stomach, one hour before breakfast.
- Iron, calcium supplements and antacids also reduce levothyroxine absorption. It should be taken 4 hours before or after taking these products.
Many medicines interfere with the absorption of levothyroxine; these include calcium supplements, antacids containing aluminum, sucralfate, iron supplements, cholestyramine, ciprofloxacin, raloxifene, and orlistat.
Some Specific Products Interfering with levothyroxine absorption
Alka-Seltzer™.
Milk of Magnesia.
Alternagel™, Amphojel™.
Gaviscon, Gelusil, Maalox, Mylanta, Rolaids.
Pepto-Bismol™.
Tums™.
Sucralfate (Carafate™)
PPIs omeprazole (Prilosec™, Prilosec OTC, Zegerid™)
lansoprazole (Prevacid™)
pantoprazole (Protonix™)
The Bottom Line
Thyroid function is variable. Absorption of medication is variable. Therefore thyroid function tests are normally done periodically to ensure appropriate levothyroxine dosing.
Anything interfering with normal stomach and intestine function can interfere with levothyroxine absorption. This includes food and many medicines, especially those that change or decrease stomach acid (e.g. heartburn meds). If one must take these, separate the dose from levothyroxine as far as possible, 4 hours would be ideal.
Is levothyroxine in a gel or liquid form better than pills?
There are 2 issues in this question. Does the inconvenience of having to take levothyroxine on an empty  stomach 1 hr. before food increase the frequency of missed doses? Are there some ingredients other than levothyroxine in pills with the potential for problems?
stomach 1 hr. before food increase the frequency of missed doses? Are there some ingredients other than levothyroxine in pills with the potential for problems?
Several studies show that a shift from levothyroxine tablets 30 minutes before breakfast to the same dose of a liquid gel AT breakfast resulted in no significant change in thyroid function tests (TSH and Free T4). However, the FDA approved package insert for Tirosint-SOL™ (levothyroxine sodium oral solution) states: “Administer once daily, on an empty stomach, one-half to one hour before breakfast. Administer at least 4 hours before or after drugs that are known to interfere with absorption.”
Information from the manufacturer of liquid levothyroxine indicates tablet levothyroxine may contain wheat starch with gluten, lactose, dyes, sugar, cellulose, mannitol, sucralose and others. They indicate Tirosint-SOL™ (levothyroxine sodium oral solution) contains only levothyroxine, water and glycerol. “Everyone is paying closer attention to the ingredients found in the foods we consume these days, so it only makes sense to do the same with medication. For people with serious food allergies or restrictions, exposure to even small quantities of certain ingredients may cause a serious reaction. In a recent survey of nearly 1,000 patients taking levothyroxine to treat their hypothyroidism, 15% of respondents reported allergies to the excipients commonly found in levothyroxine tablets” from the Tirosint-SOL™ website.
COST. Approximately $130-$140 per month retail price. A co-pay card, $15 per month is available.
